Adverse childhood experiences
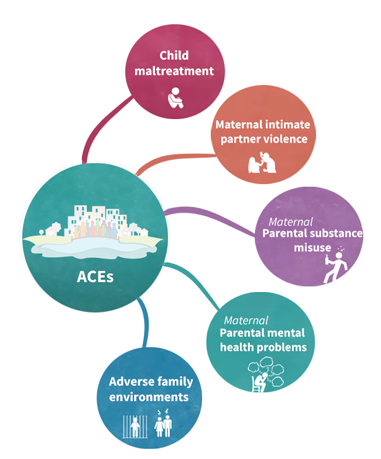 Adverse childhood experiences (ACEs) are potentially traumatic, violent, or neglectful experiences in childhood that can have a profound impact on a child’s health and development (1). Examples of recorded ACEs include child maltreatment (e.g. child protection), exposure to domestic violence, and growing up with a parent with a mental health or substance use problem (e.g. trio of vulnerabilities).(2).
Adverse childhood experiences (ACEs) are potentially traumatic, violent, or neglectful experiences in childhood that can have a profound impact on a child’s health and development (1). Examples of recorded ACEs include child maltreatment (e.g. child protection), exposure to domestic violence, and growing up with a parent with a mental health or substance use problem (e.g. trio of vulnerabilities).(2).
ACEs in EHRs
Electronic health records (EHRs) contain a wealth of routinely collected information about patients, including their medical history, medications, and social history. ACEs in EHRs is a platform that provide clinically relevant and validated indicators to identify ACEs in EHRs. These indicators are based on several studies (3, 4, 5) and inspired by the Adverse Childhood Experiences (ACE) Study, which is a landmark study that found that exposure to ACEs is associated with a wide range of health problems, including chronic diseases, mental health problems, and substance abuse.
If you are a researcher or healthcare provider, you can use the ACE indicators to identify ACEs at a population level to identify at-risk groups to inform allocation of resources, monitoring of trends and outcomes. Clinically, ACE indicators in EHRs have the potential to support streamlining workflows, assisting decision-making, and enhancing patient care. ACEs in EHRs is a valuable tool that can help to improve the health and well-being of children and families.
We hope you will join us in our mission to improve the lives of children and families affected by ACEs.
Mission statement and aims
EHRs are routinely collected and readily available. However, there are significant challenges in using EHRs to inform practice and policy about ACEs. EHRs are often stored in different databases, organisations, and coding systems. This can result in a complex and messy web of information that requires specialist data management skills to use. Another challenge is that there was no previously well-defined and validated set of indicators for identifying ACEs in EHRs using both parent and child data.
Our mission is:
- To improve the health of families and young people by using electronic health records (EHRs) to identify and measure adverse childhood experiences (ACEs).
- To advocate for early support and family centred services for families with ACEs.
- To work with researchers, professionals, and policymakers to promote trauma-informed care and public health policies that support families affected by ACEs.
- To enhance the methodological standard, accessibility, and utility of data-driven think-family approaches to study adversity using EHRs.
- To provide a validated system to measure intervenable and clinically relevant ACEs with the potential to support trauma-informed data-driven research, public health, policy, and health care.
- To continuously develop the www.ACEsinEHRs.com platform to improve resources for researchers, professionals, and policymakers.
Achievements - ACEs in EHRs:
- Developed common data standards and coding systems for ACEs in EHRs.
- Developed data management tools and resources to make ACE indicators in EHR more accessible and usable.
- Developed methods for linking and studying EHR data across families.
- Supporting research on the use of EHRs to identify and measure ACEs.
- Disseminated research findings to healthcare providers, policymakers, and the public.
All platform activity is publicly logged. All code for data management and analysis is shared under open licenses.
We follow WHO’s Minsk Declaration and view ACEs through a “life-course” and a “trauma-informed” lens. This approach acknowledges that risk is not static and depends on the interaction of multiple unmeasured promotive, protective, and risk factors throughout generations and people’s lives.
Advantages of EHRs
ACEs are preventable. However, many ACEs are very difficult to identify in childhood. Most studies rely on adults’ self-reports many years after the event and are prone to memory biases. This “time gap” also means data is collected when it’s more challenging to prevent the harmful effects of ACEs. EHRs are routinely collected data from hospitals, GPs and other health systems. The data is often recorded “prospectively” or as events happen and as part of routine care. The information is available shortly after a health care presentation and poses less burden to patients than completing a traditional research survey. All data is made non-identifiable and stored securely (watch the video below to find out more). EHRs also provide researchers with larger samples than self-report or interview-based samples.
In the UK, mothers’ and children’s EHRs can be linked across services. The ability to link mothers’ and children’s records allows for measuring ACEs before pregnancy, throughout childhood and intergenerationally.
Limitations of ACEs in EHRs
It is essential to note:
- There are methodological challenges in accurately linking children’s EHRs to their fathers’ EHRs (a long-standing issue of anonymised secondary and primary care data), meaning ACEs in EHR research have primarily been based on linked maternal and child data.
- Only identify experiences recorded in semi-structured coded non-identifiable data. Many children might have concerns recorded only in free-text data that is not captured in coded data.
- Do not represent an exhaustive list of all possible adversities experienced by children
- Cannot make inferences about an individual. This means that indicators cannot be used to guide individual-level clinical decision-making, including screening, diagnosing or labelling children or families to be at risk of harm.
- Do not assume children with ACEs will develop poorer health outcomes. Most children with ACEs do not develop poorer health outcomes and show resilience.
- Do not account for different protective factors and contexts
The limitations of the “ACE” concept have been summarised elsewhere.
Team & Contributors
This project was developed by a range of researchers and clinical experts:
- Dr Shabeer Syed, Clinical Psychologist & Senior Research Associate (s.syed.16@ucl.ac.uk), 1,2
- Dr Arturo Gonzalez-Izquierdo, Senior Research Associate, 1, 3
- Dr Linda Wijlaars, Senior Research Associate, 1, 3
- Dr Janice Allister, General Practitioner, 5
- Dr Leah Li, Associate Professor in Medical Statistics and Epidemiology, 1
- Dr Matthew Jay, Senior Research Associate, 1
- Prof Gene Feder, Professor of Primary Care, 4
- Dr Louise Johns, Consultant Academic Clinical Psychologist
- Dr Richard F Howard, Consultant in Anaesthesia and Pain Medicine, 6,7
- Prof Ruth Gilbert, Professor of Clinical Epidemiology (r.gilbert@ucl.ac.uk), 1,3
- Dr Rebecca E Lacey, Associate Professor of Life Course Epidemiology
- Prof Laura D Howe, Professor of Epidemiology and Medical Statistics
- Prof Jessica Deighton, Professor in Child Mental Health and Wellbeing
- Dr Rachel Ashwick, Clinical Psychologist
- Mr Muhammad Qummer ul Arfeen, Data Manager, UCL Institute of Health Informatics, 3
1. UCL Great Ormond Street Institute of Child Health, Population, Policy and Practice, Faculty of Population Health Sciences London WC1N 1EH 2. Oxford Institute of Clinical Psychology Training and Research, University of Oxford, Oxford, UK 3. Institute of Health Informatics and Health Data Research UK, University College London 4. Bristol Medical School, Bristol Population Health Science Institute Centre for Academic Primary Care, University of Bristol 5. General Practitioner, NHS 6. Paediatric Pain Research Group, University College London Great Ormond Street, Institute of Child Health, London WC1N 1EH 7. Department of Anaesthesia & Pain Medicine, Great Ormond Street Hospital for Children NHS Foundation Trust
Feedback & Contributions
We are continuously working to make this platform and the ACE indicators easier to access and implement. All platform activity is publicly logged. All code for data management and analysis is shared under open licenses. This website is open source and hosted via Github.
If you would like to contribute or provide feedback, please get in touch at s.syed.16@ucl.ac.uk
Acknowledgements
This webpage accompanies a study that uses patients’ data collected by the NHS as part of their care #DataSavesLives. We are extremely grateful to the generosity of the patients and their families, along with the participating GP practices and NHS staff, for their ongoing contribution to mental health and family violence research. The ACEs studies (protocols: 19_162R, 21_000587) were approved by the MHRA (UK) Independent Scientific Advisory Committee, under Section 251 (NHS Social Care Act 2006). The ACEs studies were carried out as part of the CALIBER© resource. CALIBER, led by the UCL Institute of Health Informatics, is a research resource providing validated electronic health record phenotyping algorithms and tools for national structured data sources. The ACEs studies are based on data from the CPRD obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. The interpretation and conclusions contained in this study are those of the author/s alone HES, and ONS are under copyright © (2020), re-used with the permission of The Health & Social Care Information Centre. All rights reserved. The research was supported in part by the NIHR Great Ormond Street Hospital Biomedical Research Centre. This research benefits from and contributes to the NIHR Children and Families Policy Research Unit, but was not commissioned by the National Institute for Health Research (NIHR) Policy Research Programme. The views expressed are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm’s length bodies, and other Government Departments.
More information about ACEs
For further information about research on ACEs and their uses, please visit:
- CDC
- British Psychological Society
- World Health Organization - Prevention of Violence
- University College London reports
- The BMJ
The Lancet research collections:
- Violence
- Child maltreatment
- Violence against women and girls
- Family planning
- Women’s and Children’s Health in Conflict Settings
JAMA research collections:
Policy implications related to ACEs:
Public Health England/Wales:
- Vulnerability in childhood: a public health informed approach
- Promoting children and young people’s emotional health and wellbeing
- Public Health Wales
- Public Health Wales study on routine screening of ACEs at GP practices
UK, HM Government or Home office:
World Health Organization:
Users must cite the www.ACEsinEHRs.com library and the accompanying Lancet Digital Health publication in all research outputs, presentations and reports. The information is not intended for clinical use. No data is stored in this library. Dr Shabeer Syed, Clinical Psychologist & Senior Research Associate
Go back
 |
 |
 |
 |
 |
 |
 |
 |